Treatment for DCIS
Listen to our Real Pink podcast, Impact of Diagnosis on Your Mental Health.
What is DCIS?
DCIS (ductal carcinoma in situ) is a non-invasive breast cancer. It’s stage 0 breast cancer.
With DCIS, the abnormal cells are contained in the milk ducts and have not invaded nearby tissue outside the milk ducts. (The milk ducts are canals that carry milk from the lobules to the nipple openings during breastfeeding.)
It’s called “in situ” (which means “in place”) and “non-invasive” because the abnormal cells have not left the milk ducts.
DCIS is also called intraductal (within the milk ducts) carcinoma. Some people use the terms “pre-invasive” or “pre-cancerous” to describe DCIS.
Both women and men can get DCIS.
DCIS is treated to try to prevent the development of invasive breast cancer.
Learn more about breast cancer stages and staging.
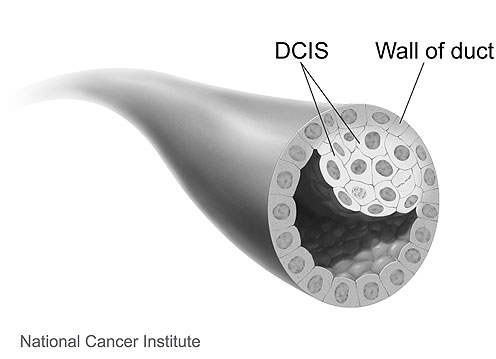 |
Image source: National Cancer Institute (www.cancer.gov) |
The following is a 3D interactive model showing DCIS. The labels show a normal duct and a duct with DCIS.
DCIS diagnosed with invasive breast cancer
DCIS can be found alone or with invasive breast cancer.
If it’s diagnosed with invasive breast cancer, treatment and the chances of survival are based on the invasive breast cancer, not the DCIS.
Learn about treatment for early breast cancer.
Treatment for DCIS
DCIS is non-invasive, but without treatment, the abnormal cells could progress to invasive breast cancer over time.
Left untreated, it’s estimated 10%-50% of DCIS cases may progress to invasive breast cancer [1-4].
Health care providers cannot predict which cases of DCIS will progress to invasive breast cancer and which will not. Because DCIS might progress to invasive breast cancer, almost all cases are treated.
Surgery is recommended as the first step to treat DCIS. After surgery, some people will have radiation therapy, and some may take hormone therapy.
Learn more about treatments for DCIS.
Learn about the risk of invasive breast cancer after treatment for DCIS.
Learn about emerging areas in the treatment of DCIS.
Watch our video of Former Komen Chief Scientific Advisor Dr. George Sledge as he shares some things to think about before getting treatment.
Your health care team
Throughout your treatment and beyond, you’ll get care from many health care providers. Your health care team may include:
- Doctors involved in cancer treatment (medical oncologists, surgeons, radiation oncologists)
- Doctors involved in other care for people with breast cancer (radiologists, pathologists, plastic surgeons and others)
- Your primary care doctor
- Nurses
- Genetic counselors
- Patient navigators
- Social workers
- Mental health providers (counselors, clinical social workers, psychologists and others)
- Dietitians
- Physical therapists
- Pharmacists
- Integrative care specialists
- Other health care providers (your gynecologist and any other specialists you see should continue to be part of your care team)
These health care providers may be involved in your care throughout diagnosis, treatment and beyond.
If you’re not happy with your care or you’re not connecting with your doctor, consider getting a second opinion. It’s OK to get a second opinion at any point during your care. Your doctor should never discourage you from getting a second opinion.
Learn about choosing a doctor.
Learn about choosing a hospital.
Learn more about getting a second opinion.
Online access to your medical information
Most hospitals and doctors’ offices now allow you access to your medical information online. You set up an account with a login name and password. This provides security to protect your privacy.
An online account gives you access to your test results, pathology and radiology reports, prescription drug information, medical appointments, doctors’ notes and more. It also gives you another way to communicate with your health care team.
Staying organized |
You’ll be getting information from different members of your health care team. So, it may be helpful to use a notebook or 3-ring binder with pockets, apps on your phone or tablet, or other organizer to keep track of your breast cancer treatments and health care team. You may want to include:
Susan G. Komen® has interactive Questions to Ask Your Doctor resources that you can download and write on that may be helpful to include. |
Treatment guidelines
Although the exact treatment for DCIS varies from person to person, guidelines help make sure high-quality care is given. These guidelines are based on the latest research and agreement among experts.
The National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO) are respected organizations that regularly review and update their guidelines.
In addition, the National Cancer Institute (NCI) has treatment overviews.
Talk with your health care team about which treatment guidelines they follow.
After you get a recommended treatment plan from your health care team, study your treatment options. Together with your health care team, make thoughtful, informed decisions that are best for you. Each treatment has risks and benefits to consider along with your own values and lifestyle.
Survival after DCIS
With treatment, the chances of survival for DCIS are usually excellent.
Learn more about breast cancer survival rates.

Thelma Brown, Komen Advocates in Science member
“A diagnosis of any stage of breast cancer can be very frightening. Often, the first instinct is to act quickly. There is not a one size fits all approach to breast cancer, and DCIS is no different. Therefore, it is important to slow down and take the time to learn about DCIS and your treatment options. This will enable you to be an active member of your health care team and share in the decision-making.”
Surgery for DCIS
Surgery is the first step to treat DCIS. It removes the abnormal tissue from the breast. It’s the main treatment for DCIS, but you may also have other treatments.
Depending on how far the DCIS has spread within the milk ducts, surgery can be a mastectomy or a lumpectomy.
If DCIS is spread throughout the ducts, affecting a large part of the breast, a total (simple) mastectomy will be done. With a total mastectomy, the surgeon removes the entire breast and possibly some lymph nodes, but no other tissue.
If there’s little spread of DCIS within the ducts, you will likely have a choice between a mastectomy or a lumpectomy.
With a lumpectomy, the surgeon removes only the abnormal tissue in the breast and a small rim of normal tissue around it (called a margin). The rest of the breast is left intact. Lymph nodes are not usually removed with a lumpectomy for DCIS.
Overall survival is the same for women with DCIS who have a mastectomy and those who have a lumpectomy (with or without radiation therapy) [5].
In the U.S., most women with DCIS are treated with a lumpectomy followed by radiation therapy [6].
Learn about deciding between a mastectomy and a lumpectomy.
Sentinel lymph node biopsy during a mastectomy for DCIS
A sentinel lymph node biopsy is a procedure used to check whether or not invasive breast cancer has spread to the axillary lymph nodes (the lymph nodes in the underarm area). The surgeon removes 1-5 axillary lymph nodes.
A sentinel lymph node biopsy is done at the same time as a mastectomy for DCIS. This helps some people avoid a more invasive lymph node surgery that removes more lymph nodes (called an axillary lymph node dissection) later.
Once a mastectomy has been done, a person can’t have a sentinel lymph node biopsy.
If it turns out there’s invasive breast cancer (along with DCIS) in the tissue removed during the mastectomy, and a sentinel lymph node biopsy wasn’t done, an axillary lymph node dissection might be needed. So, having a sentinel lymph node biopsy helps some people avoid an axillary lymph node dissection.
Radiation therapy
Standard radiation therapy (also called radiotherapy) uses targeted, high-energy X-rays or other forms of radiation to kill cancer cells.
The goal of radiation therapy is to kill any cancer cells that might be left in the breast after breast cancer surgery.
After a mastectomy
Women treated with a mastectomy for DCIS generally don’t benefit from radiation therapy. However, in rare cases, it may be recommended because of the extent or location of the DCIS.
After a lumpectomy
A lumpectomy for DCIS is often followed by radiation therapy to lower the risk of [5-12]:
- DCIS recurrence (a return of DCIS) in the treated breast
- Invasive breast cancer in the treated breast
A meta-analysis that combined the results of 4 randomized clinical trials showed adding whole breast radiation therapy after a lumpectomy reduced the risk of DCIS recurrence or invasive breast cancer (each in the breast treated for DCIS) by half compared to a lumpectomy alone [6].
Overall survival is the same for women with DCIS who have a lumpectomy with or without radiation therapy [5-7]. So, questions remain about the need for all women to get radiation therapy after a lumpectomy for DCIS.
Some women with small, low-grade or intermediate-grade DCIS and widely negative surgical margins may have a low risk of DCIS recurrence or invasive breast cancer after a lumpectomy [5]. (Low-grade and intermediate-grade DCIS tend to grow more slowly than high-grade DCIS. Margins are negative when there are no cancer cells in the rim of breast tissue surrounding the tumor that was removed during surgery.) Some of these women with a low risk may choose to avoid radiation therapy altogether or consider limited radiation therapy such as partial breast radiation therapy [5,12].
Radiation therapy for DCIS is usually given every day, 5 days a week, for 3-4 weeks.
Learn about going through radiation therapy.
Learn more about surgical margins.
| For a summary of research studies on treatment for DCIS with a lumpectomy plus whole breast radiation therapy, visit the Breast Cancer Research Studies section. |
Hormone therapy
Hormone receptor status
A pathologist determines the hormone receptor status of the DCIS by testing the tissue removed during a biopsy.
- Hormone receptor-positive (estrogen receptor-positive/progesterone receptor-positive) DCIS tumors express hormone receptors. This means they have a lot of hormone receptors. Hormone receptor-positive tumors need estrogen and/or progesterone to grow.
- Hormone receptor-negative (estrogen receptor-negative/progesterone receptor-negative) DCIS tumors do not express hormone receptors. This means they have few or no hormone receptors.
Most cases of DCIS are hormone receptor-positive. People with hormone receptor-positive DCIS may benefit from hormone therapy (tamoxifen or an aromatase inhibitor) [5,9,13-17].
Learn about hormone receptor status and invasive breast cancer.
After a mastectomy
Hormone therapy isn’t usually recommended for women who have a mastectomy for DCIS. These women have an excellent chance of survival with a very low risk of DCIS recurrence or developing invasive breast cancer in the opposite breast [5].
For women who have a mastectomy for DCIS, the benefit of hormone therapy would likely be very small and would mostly affect the risk of cancer in the opposite breast.
After a lumpectomy
The National Comprehensive Cancer Network (NCCN) recommends women who are treated with a lumpectomy for hormone receptor-positive DCIS consider taking hormone therapy (tamoxifen or an aromatase inhibitor) for 5 years [5].
In women treated with a lumpectomy and radiation therapy for DCIS, studies have shown hormone therapy can lower the risk of [5-12]:
- DCIS recurrence (a return of DCIS)
- Invasive breast cancer
These risks are lowered in both the treated breast and the opposite breast.
Low-dose tamoxifen
Women who have a lumpectomy for hormone receptor-positive DCIS and have trouble taking tamoxifen due to the side effects may consider taking low-dose tamoxifen for 3 years [5].
Learn more about tamoxifen, including possible side effects.
Learn more about aromatase inhibitors, including possible side effects.
Learn more about factors that affect treatment options.
Learn about emerging areas in the treatment of DCIS.
| For a summary of research studies on tamoxifen for treatment of DCIS, visit the Breast Cancer Research Studies section. |
Risk of developing invasive breast cancer after DCIS
After treatment for DCIS, there’s a small risk of:
- DCIS recurrence (a return of DCIS)
- Invasive breast cancer
These risks are higher with a lumpectomy plus radiation therapy than with a mastectomy [5]. However, overall survival is the same after either treatment [5].
Higher grade DCIS appears more likely than lower grade DCIS to recur as DCIS or invasive breast cancer after treatment (surgery, with or without radiation therapy) [18].
With close follow-up, invasive breast cancer is usually caught early and can be treated effectively.
Questions you may want to ask your health care provider
About your diagnosis
- Is ductal carcinoma in situ (DCIS) breast cancer? How is DCIS different from invasive breast cancer?
- Is my DCIS estrogen receptor-positive or estrogen receptor-negative?
Treatment
- What are my treatment options? Which treatments do you recommend for me and why?
- What are my chances for DCIS recurrence? What about developing invasive breast cancer?
- Should I have genetic testing before treatment begins?
- Do you recommend I have a lumpectomy (breast-conserving surgery)? If not, why not?
- If I have a lumpectomy plus radiation therapy now, and the breast cancer returns (as a DCIS recurrence or invasive breast cancer), will I need to have a mastectomy at that time?
- Talk to me about breast reconstruction if I have a mastectomy. If I decide I want reconstruction, when can I have it (at the same time as the mastectomy or at a later date)? What are the risks? What about prosthesis options? Who else should I see to discuss and plan for reconstruction or prosthesis?
- If I have a mastectomy, will a sentinel lymph node biopsy be done?
- Will I need radiation therapy after my surgery? If so, when will I meet with the radiation oncologist to discuss my radiation therapy?
- If my DCIS is estrogen receptor-positive, what are the benefits of taking a hormone therapy drug (tamoxifen or an aromatase inhibitor)?
- If I will be taking hormone therapy, what do I need to consider before treatment begins if I would like to have a child after being treated for DCIS?
- Were my tumor margins negative (also called uninvolved, clean or clear)? If not, what more will be done?
- Are there clinical trials enrolling people with DCIS? If so, how can I learn more?
- How quickly do I need to make a decision about my treatment plan?
- Will some of the tissue removed during surgery be stored? Where will it be stored? For how long? How can it be accessed in the future?
Follow-up care
- How often will I have check-ups and follow-up tests after treatment ends?
- Will a follow-up care plan be prepared for me?
- Who is in charge of my follow-up care?
Learn more about talking with your health care provider.
If you’ve been recently diagnosed with DCIS or feel too overwhelmed to know where to begin to gather information, it may be helpful to download and print some of Susan G. Komen®‘s resources. For example, we have Questions to Ask Your Doctor About Breast Cancer Surgery and Questions to Ask Your Doctor About Radiation Therapy and Side Effects.
You can download and print resources to take with you to your next doctor’s appointment or you can save them on your computer, tablet or phone using an app such as Adobe. Plenty of space and a notes section are provided to write or type the answers to the questions.
There are other Questions to Ask Your Doctor resources on many different breast cancer topics you may wish to download.
Susan G. Komen® was one of 13 organizations that sponsored the National Academy of Sciences report, Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. The report identified key ways to improve quality of care:
Read the full report. |
Clinical trials
After discussing the benefits and risks with your health care provider, we encourage you to join a clinical trial if there’s one right for you.
Susan G. Komen® Patient Care Center |
If you or a loved one needs information or resources about clinical trials, the Patient Care Center can help. Contact the Komen Breast Care Helpline at 1-877-465-6636 or email clinicaltrialinfo@komen.org. Se habla español. |

BreastCancerTrials.org in collaboration with Komen offers a custom matching service to help find clinical trials that fit your health needs.
Learn more about clinical trials.
You’re not alone
If you’ve been diagnosed with DCIS, it’s normal to feel many different emotions, including being worried or scared about going through treatment and the side effects you may have. You may also be thinking about what your life will be like after you finish treatment.
Many people have been where you are today. They had the same concerns and fears. They’ve gone through breast cancer treatment and are living their lives.
It may be helpful for you to talk about how you’re feeling and get support from others. Having people in your life who can relate to some of what you’re going through may help you feel less alone.
You could share your experience and advice with others going through treatment for DCIS or those who’ve finished treatment. You can do this in a support group or by connecting one-on-one with another DCIS survivor. A social worker or patient navigator can help you find these resources.
You can also talk with your health care providers about how you’re feeling. They care about your overall well-being and want to help They may connect you to a mental health provider on your health care team, such as a social worker, for emotional support.
Our Support section has a list of resources to help find local and online support groups and other resources.
Learn more about social support and support groups.
Learn about healthy ways to cope with stress.
Susan G. Komen® Support Resources |
|
Updated 12/23/24
This content is regularly reviewed by an expert panel including researchers, practicing clinicians and patient advocates.




